Pain Reimagined: The Science and Future of Neuromodulation
Harnessing Technology to Transform Chronic Pain Treatment
Hello everyone!
If you're new here, welcome! I recommend starting with Article 1 and Article 2 to get a solid foundation in this intriguing field.
Pain is a universal experience—whether it’s a stubbed toe, a headache, or a persistent condition, it serves as the body’s alarm system, signaling that something is wrong. But pain is more than just a sensation; it’s a complex process involving the brain and nervous system. And innovative techniques like neuromodulation offer new hope when pain becomes chronic! Neuromodulation is like adjusting the brain or nervous system’s "volume" to improve function. It involves using mild electrical signals, magnetic fields, or chemicals to help nerves work better.
Our previous article provided an overview of chronic pain and how neuromodulation can help. Today, we’re diving deeper into the science behind the neuromodulation techniques commonly used to manage it. By exploring how these interventions work, we can better understand why neuromodulation holds such promise for improving lives.
Exploring Neuromodulation Techniques
If you’ve ever dealt with pain that just won’t go away, you know how exhausting and frustrating it can be. Maybe you’ve tried painkillers, physical therapy, or other treatments with little success. This is where neuromodulation comes in—a modern approach that changes how pain signals are processed in the nervous system.
Instead of just masking pain like medication does, neuromodulation adjusts how your nerves and brain perceive pain, often providing relief where other treatments fail. Depending on the type and severity of pain, neuromodulation techniques fall into two categories:
Invasive techniques (for severe or long-term pain): These involve surgically implanting small devices that send signals to nerves or the brain to block or alter pain perception.
Non-invasive techniques (for mild to moderate pain or those who prefer a non-surgical approach): These use external devices, like skin electrodes or magnetic stimulation, to reduce pain without requiring surgery.
Invasive Neuromodulation Techniques: When You Need Stronger, Longer-Lasting Relief
Invasive techniques are for people who have tried everything else—medications, physical therapy, even surgery—and still struggle with constant, life-altering pain. These methods work by delivering controlled electrical pulses to nerves or the brain, essentially retraining the nervous system to process pain differently. Here are some examples:
Spinal Cord Stimulation (SCS) – “Rewiring” Pain Signals at the Source
Best for: Chronic back pain, nerve pain after surgery, complex regional pain syndrome (CRPS).
How it works: Think of your spinal cord as a highway for pain signals. SCS puts a “roadblock” on that highway, so pain messages can’t travel up to the brain as strongly.
How it’s done: A small device (similar to a pacemaker) is surgically placed near the spine, with tiny electrodes sending mild electrical pulses to disrupt pain signals.
Why it matters: If you have severe back or nerve pain that hasn’t improved with surgery or medication, SCS can significantly reduce discomfort and help you rely less on painkillers.
What does it feel like? Instead of pain, most people describe a gentle tingling or warmth in the affected area, which is much easier to tolerate than chronic pain.
Peripheral Nerve Stimulation (PNS) – Targeting Pain at Its Source
Best for: Localized pain (like in the arms, legs, or face), nerve injuries, migraines.
How it works: If SCS is like a highway roadblock, PNS is like rerouting traffic in a single neighborhood—it focuses on specific nerves that are causing pain.
How it’s done: Tiny electrodes are implanted near the affected nerve, sending mild pulses to “trick” the nerve into reducing pain signals.
Why it matters: If you have pain in one particular area—such as after surgery or due to nerve damage—PNS is a more focused approach than SCS.
What does it feel like? Since the stimulation is localized, many people say the relief feels more naturalbecause it matches their exact pain area.
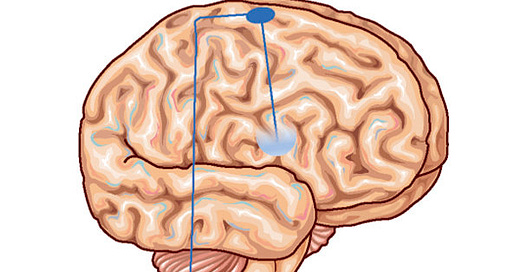
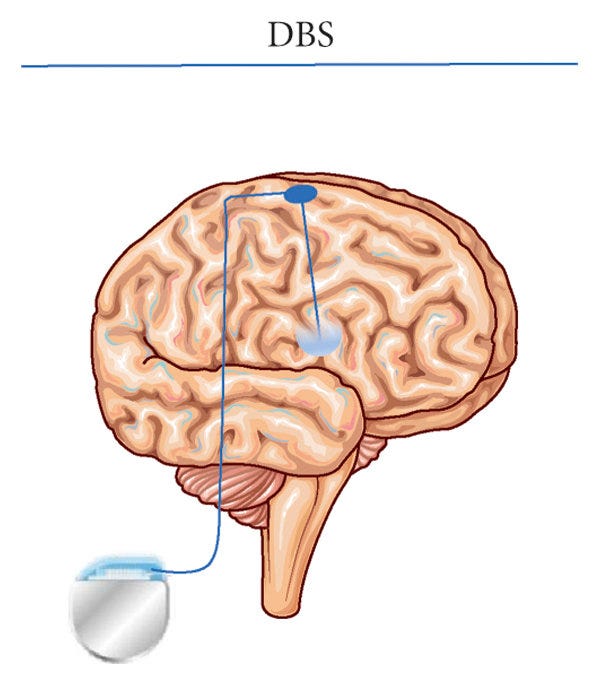
Deep Brain Stimulation (DBS) – Calming the Brain’s Pain Centers
Best for: Severe, treatment-resistant pain, nerve disorders, Parkinson’s-related pain.
How it works: DBS directly targets pain-processing areas of the brain, adjusting how they interpret pain.
How it’s done: Electrodes are surgically placed inside specific brain regions, and a small device delivers electrical pulses to reduce overactive pain signals.
Why it matters: This is a last-resort option, used when other treatments have failed. If pain severely limits your life and no other neuromodulation method works, DBS can provide relief.
What does it feel like? Patients don’t feel the stimulation itself but notice a gradual reduction in pain intensity over time.
Figure from Biase et al., 2021
Non-Invasive Neuromodulation Techniques: A Gentle, Surgery-Free Approach
If the idea of implanting a device sounds overwhelming, non-invasive neuromodulation offers an easier way to try pain relief. These techniques use external stimulation (electrical, magnetic, or radiofrequency pulses) to alter pain signals—without surgery. Here are some examples:
Transcutaneous Electrical Nerve Stimulation (TENS) – A Drug-Free, At-Home Option
Best for: Muscle pain, arthritis, joint pain, post-injury recovery.
How it works: TENS uses a small, portable device with sticky skin electrodes that send gentle electrical pulses to nerves. This confuses pain signals before they reach the brain.
Why it matters: If you have aches, muscle tension, or arthritis pain, TENS is a simple, drug-free way to get quick relief at home.
What does it feel like? A mild tingling or buzzing sensation—many people find it relaxing!
Image by Johnson 2021
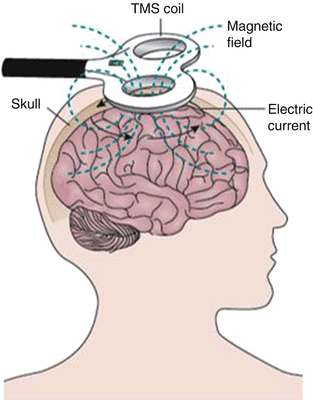
Transcranial Magnetic Stimulation (TMS) – Using Magnetism to Reset Pain Perception
Best for: Migraines, neuropathic pain, conditions where pain is linked to brain activity.
How it works: A device places a magnetic coil near the scalp, which gently stimulates the brain areas involved in pain processing.
Why it matters: If your pain comes from neurological conditions (like migraines or nerve pain) rather than physical injuries, TMS can help reset pain perception.
What does it feel like? A light tapping sensation on the scalp, but no pain.
Figure from McClelland, J. (2017)
Pulsed Radiofrequency (PRF) – A Longer-Lasting Pain Relief Option
Best for: Nerve pain (like sciatica), joint pain, herniated discs.
How it works: PRF sends low-energy radio waves to targeted nerves, modifying how they transmit pain—without damaging them.
Why it matters: If you need longer-lasting relief than TENS or TMS, PRF can provide months of pain reduction after just one session.
What does it feel like? A mild warmth, with gradual pain relief over the following weeks.
How Do You Choose the Right Technique?
If you’re struggling with chronic pain, you might wonder: Which neuromodulation approach is right for me?
Mild to moderate pain? Try non-invasive methods like TENS, TMS, or PRF for convenient, low-risk relief.
Severe or long-lasting pain? Invasive options like SCS, PNS, or DBS might be better if you need stronger, longer-lasting relief.
Pain in a specific body part? PNS or PRF might be ideal for targeted relief.
Pain that hasn’t responded to anything else? DBS is usually a last resort for the most complex cases.
Ask your doctor – the above suggestions aren’t exhaustive, and research continues to uncover new approaches. Be sure to discuss your specific condition, goals, and medical history to determine the best option for you.
Why Should You Care?
Pain isn’t just a physical sensation—it affects your mood, energy, sleep, and overall quality of life. If pain is interfering with your daily activities, neuromodulation offers real hope. By changing how the nervous system processes pain, these techniques help people regain control over their lives, often reducing the need for medications that come with side effects.
With advancements in neuromodulation, pain relief is becoming more personalized, effective, and accessible than ever before. Whether through a small wearable device or an implanted system, these innovative treatments are helping people move past pain and get back to living.
About me!
I'm Aditi Doshi, a fifth-year Ph.D. candidate in Neuroscience. My research in non-invasive neuromodulation ignited a passion for translating cutting-edge research into practical applications. NeuroPulse Chronicles, my neuromodulation-themed newsletter, aims to raise awareness about the field and technologies designed to improve lives.
In upcoming newsletters, we'll explore various neuromodulation techniques, comparing their benefits, limitations, and accessibility challenges. I'll also highlight the companies and breakthroughs shaping the future of neuromodulation for chronic pain—from established manufacturers to cutting-edge startups—shedding light on the innovations transforming patient care.
Subscribe and Stay Informed
If you still need to subscribe, now is the perfect time. Join me on this quest to unravel the mysteries of neuromodulation, and together, let's shine a light on the incredible potential within our brains.
Thank you for being part of the NeuroPulse community!
Cheers,
Aditi Doshi